We’re excited to share that Rexera, a Z21 Ventures portfolio company, has been acquired by RealPage, a market leader in property management technology. This milestone is not just a testament to Rexera’s execution, but to the broader shift underway as legacy industries begin their transition to AI-native operations.
Rexera didn’t just ride the AI wave. It rebuilt the research and execution stack for an industry long overdue for modernization.
From Traditional ML to Agentic AI
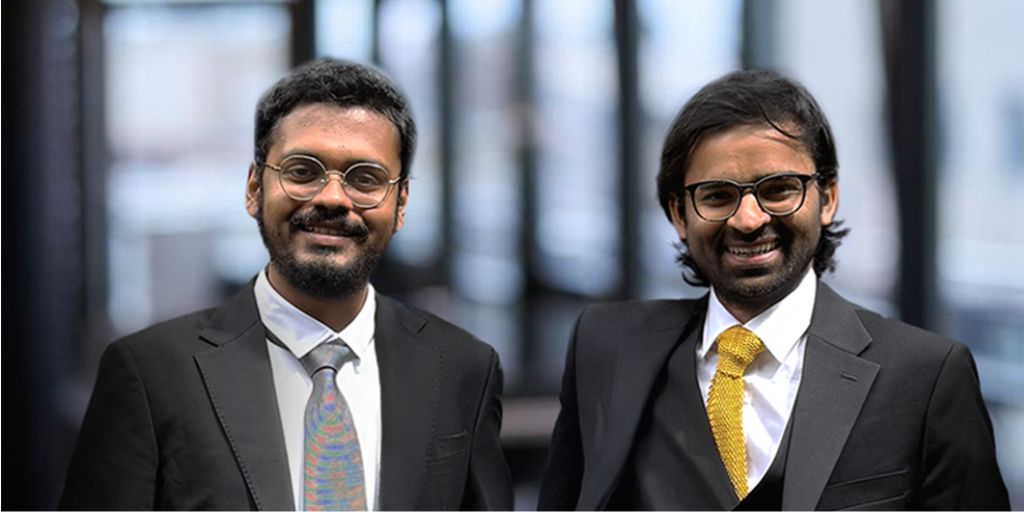
Founded by Vishrut Malhotra, Anton Tonev and Atin Hindocha, Rexera set out to accelerate real estate transactions, a process historically slowed down by paperwork, emails, and fragmented operational workflows. In its early days, Rexera relied on traditional machine learning to automate repetitive tasks like document parsing and email generation.
But as the team ventured deeper into the real estate transaction lifecycle, they encountered a fundamental limitation. Traditional ML systems were not capable of handling workflows that required human-like reasoning and contextual judgment.
The inflection point came with the emergence of large language models (LLMs). Recognizing their potential early, Rexera pivoted decisively, not just to LLMs, but to a full-fledged agentic architecture. The team built a platform powered by eight specialized AI agents, each responsible for a distinct operational function: reading documents, replying to emails, making phone calls, running QA checks, and more. These agents worked together to execute complex workflows end to end.
What followed was a deep technical reinvention. Rexera introduced its own software development methodology, the Agent Development Lifecycle (ADLC), inspired by probabilistic modeling techniques from quantitative finance. Unlike deterministic systems, LLMs required a new approach to architecture, training, deployment, and iteration. Adapting to this shift wasn’t trivial. The company had to rebuild its engineering team, onboarding junior talent trained from scratch in ADLC, as traditional mid-senior engineers struggled to adapt.
Despite headwinds in the real estate market, Rexera grew to serve over 150 customers, from large national title firms to boutique lenders. It now powers nearly 1% of real estate transactions in the U.S.
Scaling with RealPage
The acquisition by RealPage opens up a new chapter. As RealPage embarks on its own transformation from SaaS to AI-native, Rexera’s platform will accelerate the automation of operational workflows across its customer base.
The transition has been executed thoughtfully. Rexera will retain its brand and team, including its human-in-the-loop function, and operate within RealPage. This ensures continuity in culture, product direction, and execution velocity.
Equally important, the acquisition delivered meaningful financial outcomes for the Rexera team, including equity holders within its operational workforce. For many, it was a life-changing event. It’s a reminder that impactful outcomes in venture go far beyond cap tables.
A Conversation with Vishrut
We sat down with Rexera’s founder to reflect on the journey, the tech, and what’s next.
Jyotika: What was the core product and insight behind starting Rexera, and how did it evolve?
Vishrut: Our mission from day one was simple: accelerate real estate transactions. The process is traditionally slow and manual. We started with basic ML to extract data and automate email workflows, but it quickly hit a ceiling. Real estate operations require reasoning, judgment, and context and traditional ML couldn’t handle that. Once we saw GPT-3.5 in action, we knew LLMs were the unlock. That insight drove us to build agentic AI workflows that could truly automate complex operational tasks.
Jyotika: What made building AI-native products so technically challenging?
Vishrut: LLM-based systems are probabilistic, not deterministic and that changes everything. We had to rethink how we built software. That led us to develop the Agent Development Lifecycle (ADLC), which borrows ideas from quantitative finance. But the real challenge was talent. Mid-senior engineers trained in traditional SDLC struggled with this new paradigm. So we rebuilt the team, hiring one senior leader and training junior engineers from scratch on our ADLC approach. It wasn’t easy, but it worked.
Jyotika: How will Rexera scale post-acquisition, and what does this partnership with RealPage unlock?
Vishrut: RealPage is a market leader in property management technology, powering software for over 24 million housing units worldwide. With dozens of operational workflows, the company is now undergoing its own transformation from SaaS to AI-native. That makes it the perfect home for Rexera. We’ll get to deploy our platform at enterprise scale with full support, while also learning from RealPage’s deep engineering talent. The team is intact, the brand is intact, and the vision is intact. We’re just getting started.
Jyotika: What’s next for you, and what sectors in AI or vertical SaaS are you excited about?
Vishrut: Right now, I’m fully focused on scaling Rexera within RealPage, and I see incredible opportunities to build here for many years. But over time, I’d love to bring our agentic systems approach to other legacy industries like healthcare, legal and auditing. These are massive sectors with high-friction workflows, and I think they’re ripe for true AI-native innovation. I expect we’ll see multiple category-defining companies built in these spaces in the next few years.
From z21, With Pride
At Z21, we backed Rexera early because we believed in Vishrut’s ability to execute with technical rigor and clarity of vision. Through product pivots and market cycles, he led with conviction, humility, and a sharp focus on long-term value. We are proud to be one of Rexera’s early backers, not just with capital, but with belief.
“You weren’t career VCs, you’ve been close to founders through your own journeys. That made a big difference. Every conversation with you and Raj gave me energy,” he shared. “You made me believe when the journey felt uncertain,” Vishrut shared.
We’re proud to have been part of this journey. The Rexera story is a powerful example of what’s possible when deep tech meets a vertical problem, and when a founder commits to first-principles thinking even in the face of complexity.